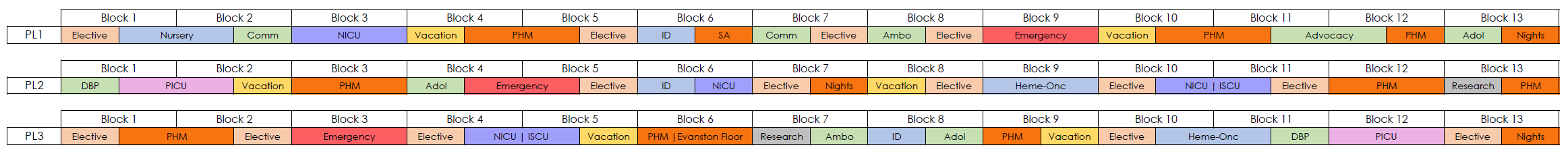
Core Pediatric Residency Block Diagram
Conferences are held twice a day Monday through Friday. Our educational series includes a mixture of the classic morning report style led by the Chief residents, lectures from fellows and attendings on core pediatric topics, interdisciplinary lectures from pharmacy and therapy services as well as a variety of resident-led education.
On Thursdays, residents attend Pediatric Grand Rounds where they meet national and international experts presenting on a range of topics from basic science and translational research to cutting edge clinical advances, to controversial topics in health policy and medical ethics.
We have a variety of other conferences that focus on wellness topics including our Restorative Justice series, Health Equity Rounds, and Ethics discussions. Throughout the year we also offer a Primary Care Series and a Scholarship Curriculum, in order to provide residents with a well-rounded experience.
Conferences are held both in person and on zoom. This time is protected for learning with pagers being handed off to the Chief Residents for triaging.
The heart of the residents’ learning comes from daily clinical teaching on the various rotations. For the inpatient rotations, including the intensive care rotations, daily teaching rounds provide dedicated time for faculty and fellows to collaborate with the residents to assure optimal care for our patients. These rounds focus on patient care decisions including the physiology and rationale behind making those decisions. Though the faculty are present and contribute significantly in all rounds, our senior residents are encouraged to be the active leaders on the teams.
In collaboration with the UC Sim Center our residents have numerous opportunities to hone their clinical skills in a safe and supportive environment. From technical skills practice of common procedures (IV placement, lumbar puncture), to resuscitation skills training in our NRP and PALS courses, to running “mock codes” in actual patient care areas throughout the hospital, our residents receive well rounded rigorous training in managing acutely ill and injured children so that they can be confident of their skills with actual patients.
Started in 2005, the Residents-Are-Teachers curriculum aims to continually expose the residents to teaching skills and opportunities for practice throughout their three years of training. Through a longitudinal, progressive curriculum, the residents gain a foundation for educational excellence.
Beginning in the intern year, there are four interactive sessions that introduce core practice topics in medical education: Giving Feedback, Teaching on Notes and Exams, the One Minute Preceptor, and Teaching at the Bedside. These sessions offer opportunities for skills practice as well as reflection on their own experiences. Second and Third years receive training in Setting Expectations/Establishing the Learning Climate, Supporting the Struggling Learner, Teaching on the Fly, and Advanced Feedback Skills. In the winter of the second year, PGY2s complete Observed Structured Teaching Encounters (OSTEs), where they engage with standardized learners and receive feedback from faculty facilitators.
Finally, for those who are interested in further developing the skills to be successful as an academic educator, we offer a two-week intensive Teaching Elective, an opportunity to apply for the GME track of the MERITS program in medical education, and an opportunity to obtain an MHPE degree through our Scholarship Track in Medical Education.
With all the emphasis on teaching skills, it’s imperative that our residents have the opportunity to practice some of the non-clinical methods of teaching. During each year, the residents give at least one presentation. In first year, residents do a journal club presentation in groups of two to three around a journal article usually paramount to pediatrics. First years also do a presentation on a primary care topic based on the Johns Hopkins Pediatrics Ambulatory Care curriculum. For both journal club and the primary care topic presentations, first years are paired with faculty preceptors. In second year, residents give a case presentation, focusing on a patient or topic of their choosing. In third year, residents again give a case presentation, and expand on the clinical pathological correlation on the topic of their choosing. Many of the second and third year residents invite faculty members of various specialties to attend the conference and add an expert opinion to their talk.
Third-year residents also have the opportunity to provide structured bedside teaching and didactic sessions for medical students while on the Float rotation.
Amidst a pandemic disproportionately affecting communities of color and a national reckoning with centuries of systemic racism and structural violence, we believe it is vital that physicians understand the context from which our patients present. Structural competency is defined as “the diagnostic recognition of the social, economic and political conditions that produce health inequities in the first place.” Situated in an underserved area within a deeply segregated city, we seek to partner with our community to understand institutional, systemic, and medical racism in order to better serve our patients.
While this is a resident-curated curriculum, we mindfully prioritize involvement of members, organizations, and experts of our community to teach us whenever possible. Sessions occur regularly, with past topics including (but not limited to): the history of Chicago's segregation and UChicago's role in the community, community asset mapping, environmental racism, immigrant and LGBTQi health, and various medical topics specific to black and brown bodies.
Our dedicated PCC didactics are embedded during our morning and noon conferences, providing our residents with attending-led, practical education and training. From our inaugural PCC lecture on the importance of building trust as leaders of the medical home by alumni Dr. Sameer Vohra (2015), MD, JD, MA, Director of the Illinois Department of Public Health, to training on oral health and fluoride varnish application, and how to provide care for unaccompanied immigrant minors – our PCC provides breadth and depth to a variety of high yield primary care topics. We further augment this live teaching with monthly asynchronous didactic modules and board preparation questions.